Change is urgently needed
Below are some of the urgent challenges in the healthcare system facing people with lung cancer with solutions to help. Read our joint report, Start Asking the Right Questions About Lung Cancer, for more detail on why these issues require immediate attention.
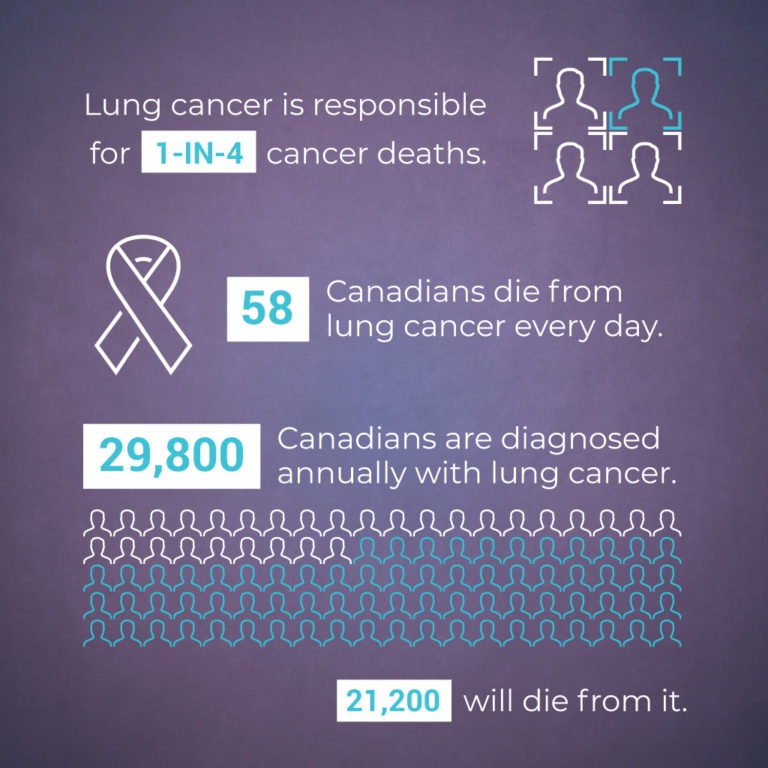
Over 80% of Canadians with lung cancer will die within five years of diagnosis. We can do more to save to more lives.
We need to increase access to screening programs to find lung cancer sooner while curative treatment is still possible.
About 70 per cent of lung cancer is diagnosed at a late stage, when it’s resistant to treatment and incurable – in part because Canadians don’t have widespread access to screening programs. All provinces and territories should expand current cancer screening programs to include lung cancer for those at higher risk.
We need to increase how fast people are diagnosed to ensure valuable time is not lost waiting in the system.
Rapid-diagnosis assessment programs (also known as diagnostic assessment programs) are the most efficient and effective way to diagnose lung cancer. However, not all Canadians have access to them. All provinces and territories should have these programs widely-available and include a patient navigator to help patients through the often complex and confusing health system. Rather than endure an agonizing wait of months filled with tests and multiple doctor referrals to multiple specialists, that time will be better spent undergoing potentially life-saving treatment.
We need to increase access to molecular testing to give people with lung cancer the most effective treatment possible.
Lung cancer is not a single disease but actually dozens of diseases, each with their own molecular variation. Identifying those variations through molecular testing can open up new cancer-fighting possibilities in the form of targeted therapies. However, Canadians struggle to get molecular testing because of challenges approving, reimbursing and accessing tests. Also, regulatory and administrative processes are not standardized and not keeping pace with innovation in cancer treatment. The federal government should develop a national molecular testing framework to guide provinces and territories on how to improve access to testing for Canadians with lung cancer.
We need faster approval of funding for medication and treatment proven safe and effective.
The time between when a drug is approved federally to when provinces and territories approve public funding is two-to-five years. That’s too long. People are quite literally dying waiting for medication that could help them. Because each province and territory independently approves which drugs they will pay for, potentially life-saving treatment is not always available equally across the country. The pan-Canadian Pharmaceutical Alliance should speed up how long it takes to negotiate drug prices and develop a system to shorten the wait times that is aligned with related review processes by the Canadian Agency for Drugs and Technologies in Health.
We need to lower the cost of lung cancer medication so everyone has access, regardless of income.
Canadians in some provinces and territories get oral cancer medication for free, while those living elsewhere have to pay for it. A person’s age can lead to high costs too. The high cost and unequal access of lung cancer medication means some Canadians have a better fighting chance because of where they live or how much money they make. It’s unacceptable. All provinces and territories should develop and expand their home cancer drug programs so all Canadians can equally access oral cancer drugs, regardless of age or income.
We need to ensure Canadians living in all areas of the country have equitable access to lung cancer care.
Often, those in Canada’s larger cities have more access to cancer treatment than those in remote areas. Canadians unable to access treatment where they live must temporarily move or regularly travel as far as six-to-10 hours away, forcing the patient and their caregivers to take substantial time off work while racking up significant travel costs. All Canadians should be treated as close to home as possible with the same standard of care. To do so, health systems need to identify and increase resources for community hospitals and regional centres that can support excellent cancer care.
We need to improve access to mental health services and social support for people with lung cancer, their families and caregivers.
Lung cancer often brings fear, stress, anxiety and depression. New symptoms, spreading cancer and side effects from treatment can make it all even harder to endure. Receiving mental health care and social support is vitally important. However, not everyone has access to it in combination with medical treatment. People diagnosed with lung cancer should be screened for distress with a clinically-validated tool. Those who are in distress should be referred for additional care relevant to their needs.